- Roux-en-Y /RNY Gastric bypass
- One anastomosis Gastric bypass OAGB /MGB
- Total revision of RNY Gastric bypass for weight gain
- Conversion of gastric bypass to Banded gastric bypass for weight gain
- Conversion of OAGB to RNY gastric bypass
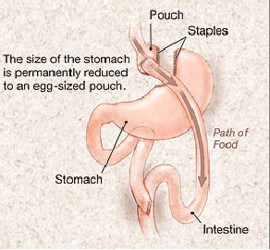
Roux-en-Y Gastric bypass or RNY Gastric Bypass RYGB involves creating a thumb sized 12-15cm long stomach pouch, as well as a bypass of most of the stomach and a varying amount of small intestine. In Roux-en-Y gastric bypass, the Biliary Pancreatic Limb BP is about 100-150cm and the Alimentary limb could be 100 cm.
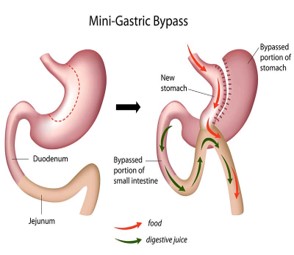
One Anastomosis Gastric Bypass OAGB/Mini-Gastric Bypass MGB or Omega Loop Gastric Bypass is basically bringing a loop of small bowel (Jejunum) and joining to Gastric pouch half the gastric bypass in that there is no Roux-en-Y formation of the gastric bypass. A loop of small bowel about 150-200cm from the Duodeno-jejunal Flexure is joined to a long (20cm long) gastric pouch, without creating the RNY configuration, to create a 150-200cm afferent limb (Biliary Pancreatic limb). No further attempt is made to divert the bile and pancreatic juices away from the gastric pouch. Some of the patients have severe nausea from the bile reflux into the stomach pouch/severe heartburn and the OAGB has to be converted to Roux-en-Y gastric bypass.
Long Pouch RNY Gastric bypass (LP-RYGB) or Diverted OAGB (D-OAGB) : To give the same effect of the restriction as in MGB/OAGB, but to prevent biliary gastric reflux and its associated problems of severe nausea and sometimes pain in abdomen and sometimes Reflux GORD, the gastric pouch is made long as in MGB/OAGB and then adding RNY configuration. This seems to give good results, though there is a slight increase in the ulcer formation than in small pouch RYGB.
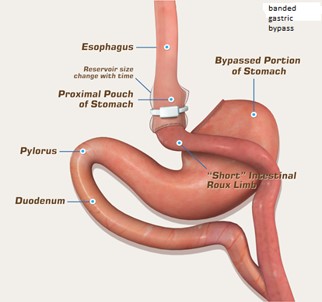
Banded Gastric Bypass: It is one of the problems of gastric bypass or any other bariatric surgery that they put on weight about 3-5 years after surgery. This is because the stomach ‘pouch’ starts stretching with time and with that the ‘stoma’ or the join between the stomach pouch and the small intestine and finally the small intestine just beyond the stoma or gastrojejunal anastomosis. To prevent this stretching of the stoma and therefore the rest of the small intestine, the silastic ‘ring’ is placed more than 2 cm proximal to the stoma /gastrojejunal anastomosis. By doing so the stomach pouch size is not changed but the stoma size/stoma will be the same unless the ‘band’ or ‘ring’ erodes through into the stomach. This erosion of the band can happen in about 2 % of patients over 15 years. If it happens, the restriction is gone from the ‘band’ and ‘band’ has to be removed using a camera (gastroscopy) into the stomach. The other problem is intolerance to food from the ‘ring’. Sometimes diagnostic laparoscopy has to be performed to release the adhesions or even remove the ‘ring’. The results at 15 years seem to be good, especially in higher BMI patients. The weight loss is maintained at the 3 year level itself which could be around 70% of their excess weight. Various authors already have presented their experience.
As a result of the re-routing of the bowel, weight loss is accomplished both by restriction of food and by malabsorption of some nutrients. Most people report diminished appetite after gastric bypass, as well as a change in the taste of food. The changed configuration interferes with the normal digestion of food. This is so because the digestive enzymes normally produced in the stomach, liver, pancreas and upper small intestine continue to be made, but do not contact the food that has been ingested until a few feet down the intestine. Hence, the digestion of the food is delayed until it is already part way down the intestine. These are additional ways the gastric bypass causes weight loss. Also we now know that the insulin-sensitizing and appetite reducing hormones like GLP1 and PYY are produced more and the insulin- resistant and appetite causing hormones like Ghrelin are produced less; because of this, metabolic syndrome is reversed. OAGB is more malabsorptive procedure than RNY gastric bypass (so expect more nutrition problems) and the weight loss could be about 60-70% excess weight, similar to or even better than gastric bypass.
Advantages of Laparoscopic Method: The advantages of performing the gastric bypass laparoscopically are that it yields cosmetically superior results and the recovery is faster. Some long-term problems, such as incisional hernias, also occur less frequently. Sometimes previous abdominal surgeries make the laparoscopic technique difficult or impossible, because of adhesions (scarring), so the open procedure may have to be resorted. Laparoscopic gastric bypass takes less than an hour to perform and routinely necessitates a stay of 1-2 days in the hospital.
Benefits:
1. Weight loss commonly reaches 70% of a person’s excess body weight. As in all weight loss surgery, however, the amount of weight loss is not guaranteed. The amount of weight a patient loses depends not only upon the surgery, but also upon what the patient does with the surgery. The surgery is not a cure for morbid obesity; it is merely a tool. Patients have been known to ingest large quantities of high caloric foods that can result in less than satisfactory weight loss. If a patient adheres to the diet, and if exercise becomes a part of the patient’s regular routine, a substantial weight loss usually results.
2. After losing this amount of weight, patients usually feel physically and mentally better. Preoperative comorbidities such as diabetes, hypertension, stress incontinence, back pain, knee pain, heel pain, sleep apnoea and other complications of obesity are usually either improved or eliminated altogether. Diabetes may disappear within a day to 6 weeks after the surgery. That’s why it is regarded as one type of metabolic surgery. Back pain may get worse if one doesn’t do exercises.
Risks:
Apart from general risks, there are some specific risks pertaining to gastric bypass
1. Operative: The main risk is the leak from the join or staple line. This causes peritonitis which requires further surgery and intensive management. It is usually noticed in the first 24 hours when there is excessive pain noticed by the patient. This can happens in less than 1 in 200 to 1:3000 cases; less if surgeon has done few hundred operations (It hasn’t happened in 3,000 primary gastric bypasses). Risk of Bleeding is much less than in Sleeve gastrectomy. Gastro-oesophageal Reflux GORD almost disappears in Roux-en-Y gastric bypass RYGB. RYGB is preferred to OAGB if there is a history of GORD
2. Late:
A. Vitamin and Protein Deficiencies. Following RNY surgery, patients are at risk of developing anaemia because of poor absorption of vitamin D, iron and vitamin B12. Therefore, dietary supplementation of these nutrients is required. The deficiencies of these are much more pronounced in OAGB and so these have to be taken in higher quantities. Exercises are important to prevent bone demineralisation. Protein supplementation is necessary especially in the first 6 months and if required after that. People require almost 60-90gm of protein a day postoperatively.
B. Difficult to evaluate excluded stomach and bowel. Since the staples at the top of the stomach completely block off the lower portion of the stomach and the upper small intestine (in the RYGB more than OAGB), there is no easy way to evaluate these portions of the gastrointestinal tract should a problem — such as ulcer, bile duct stones, or cancer — arise at a future time. In fact, although this could be a very real problem, it seldom becomes an issue.
C. Dumping Syndrome (Early). Dumping Syndrome is a condition that can cause unpleasant symptoms such as diarrhoea, nausea, light-headedness, cold sweats, weakness, tiredness, fast heart rate and stomach cramping. Light-headedness is the worst of all and one has to lie down for a while before one recovers. This occurs in the gastric bypass patients when foods especially concentrated sugars pass too quickly from the stomach into the small intestine. Dumping Syndrome can be caused by eating foods high in sugar or fat, or by drinking liquids and solids together after gastric bypass surgery. Regardless of the surgery, foods high in sugar and fat content are discouraged due to the high calorie content.
D. Hypoglycemia (Late Dumping). Low sugar levels result if high carb/calorie dense foods are eaten. This is resolved the moment these foods are avoided. Hypoglycaemia can result in dizziness/fainting with sweating and collapse. You may need sugar or sugary food to bring your sugar levels up to improve the symptoms. You should change the way you eat avoiding the high carb diet. If it doesn’t help, you may need medication or even surgery to reverse the gastric bypass.
E. Nausea/Vomiting/Pain. This is often caused by eating too much or too fast. Following surgery, patients will not be able to eat the quantity of food they presently eat. Be sure to eat in a slow and calm manner. Make sure to chew well and stop eating the moment one feels full. ‘20-20-20’ formula (chew 20 times, wait for 20 seconds and get up after 20 minutes) is a good one remember. Other causes of nausea and vomiting include ulcers or stricture, as well as drinking liquids with foods, and not chewing or blenderizing foods well enough. If vomiting, nausea or pain persists, contact your doctor to rule out ulcers or stricture (narrowing); you may need Gastroscopy (camera examination) or barium swallow x-ray examination.
F. Hair Loss Hair. Hair loss is a side effect of weight loss surgery. You may not see hair loss initially. Often it takes several months after surgery for hair loss to begin. Hair loss should resolve when weight and nutritional intake stabilizes. Hair loss can occur from a low protein and zinc/selenium intake, and a severe decrease in overall nutrition. It is important you eat foods high in protein and take a daily multivitamin/mineral supplement which provides a source of zinc. You most likely require protein supplement in the first 3-6 months.
G. Constipation. Constipation after gastric bypass surgery and restrictive procedures is common and should be prevented. Decreased intake of food, fibre and fluid along with iron and calcium supplementation can lead to constipation. 1. Drink plenty of fluid. 2. Exercise regularly. 3. Try baby food prunes or unsweetened prune juice, applesauce or oatmeal. 4 Once you start on a regular diet, you can start eating high fibre foods; Chew all fibre-containing foods to a paste consistency. 5. Drink plenty of fluids when increasing fibre in the diet. Also you can take Psyllium Husk 2 capsule or 2 TSF twice a day. You may require a laxative like Movicol in addition for a short period.
H. Food Intolerance. Some common problem-foods are red meat, bread, pasta, rice and the membrane of citrus fruits especially in the first 3-6 months. Toasted brown bread is better tolerated than untoasted bread. Red meat should be tried last; it may take a year before one tolerates it. Red meats are high in muscle fibre, which are difficult to separate even with a great deal of chewing. Always be very careful and chew well. Bread, Rice, Chapati and potato swell and get sticky and don’t move and therefore they are avoided for a long time.
I. Loss of Muscle Mass. Loss of muscle mass can occur after weight loss surgery, but it is preventable. It is very important to exercise after surgery. After weight loss surgery, the body is trying to combat starvation and will consume unused muscle for energy and you will lose muscle mass and strength. It is important to start walking and do small weight as soon as you go home. Always follow your physician’s advice on when to exercise; you can do most exercises within a week and swimming within 2 weeks.
J. Peptic Ulcers/Strictures/Perforation can occur at the stoma – join of the stomach pouch and the small intestine (jejunum). That’s why you are on PPIs, the acid reducing medications (Omeprazole, Lansoprazole etc.) at least for a year (you may have to continue if you are on NSAIDs like Ibuprofen); these will prevent the ulcer coming and consequentially stenosis (narrowing) or perforation (bursting of ulcer). If you get burning pain in the top of your abdomen, you should start on these medications straight away and get your doctor to organise for endoscopy (gastroscopy) to rule out ulcer. You should stop smoking as this is the most common factor for persistent marginal ulcer.
K. Internal Hernias – Mesenteric and Petersen’s and adhesions induced hernias – can occur though rarely as these defects are routinely closed. Sometimes adhesions/scars can cause intestinal obstruction. If you get abdominal pain on eating on a regular basis, you require immediate attention from your bariatric surgeon who can organise for a ‘look in’ (laparoscopy) the abdomen to find these hernias as other modalities of investigations may not find this and so surgical intervention to repair may be delayed with consequent disastrous results.
L. Weight gain. You may start putting on weight if you are not careful with your diet. The stomach pouch along with the ‘stoma’ or the ‘join’ to the small intestine and the small intestine itself will enlarge and accommodate great amount of food and therefore there is a danger of putting on weight. That’s why follow up with the bariatric surgeon and /or dietitian is essential. Applying a ‘ring’ around the gastric pouch prevents the stretching of the gastric pouch
M. Gallstones. Some develop symptomatic gallstones and the gallbladder may have to be removed.
N. Kidney Stones: Kidney stones can develop especially if one doesn’t drink enough fluids.